Co-occurring mental health and substance use disorders are common, are harmful to people’s wellbeing and social functioning, and are associated with disproportionately high costs to healthcare systems 1-9. The prevalence of co-occurring disorders in mental health (MH) and Alcohol and other Drug (AoD) treatment settings is sufficiently high that they are described as an ‘expectation rather than an exception’ 3.
There has been rapid development of psychosocial interventions for co-occurring disorders in recent years and valuable insights have been identified and built into clinical guidelines and into services’ redesign processes 9-15. As a result, an integrated care approach (coordinated treatment of both MH and AoD conditions by clinicians or services working together) is recommended as best practice because it more consistently results in better outcomes than approaches that treat these conditions separately 10,11,16-18. Despite the benefits of integrated care, such as reduced symptom severity and fewer acute-care admissions for people who have co-occurring disorders, most MH and AoD services operate independently of each other. This is problematic given that neither recognition of the need for improved clinical services nor the identification of integrated care as the preferred treatment approach (in clinical guidelines in multiple countries), has been enough to achieve meaningful and sustained change in the delivery of integrated care 3,6,8,15. Reports estimate that less than 12% of people with co-occurring disorders receive treatment for both conditions 15,19.
Identifying a clinical issue
Consistent with the research evidence, clinicians at the North Coast Mental Health Rehabilitation Unit, MNCLHD and the Coffs Harbour Drug and Alcohol Service, MNCLHD identified that up to 70% of residents of the rehabilitation unit had substance use disorders, but less than 10% of those consumers took up referral to the AoD service following discharge from the rehabilitation unit. To increase the number of people receiving AoD treatment, clinicians formed a working group to collaboratively adapt their clinical practices to be more inclusive and accessible to consumers. A research advisory group was established to provide evaluation support and to ensure practice changes were aligned with research evidence. Members included key managers and clinicians, plus representatives from the National Drug and Alcohol Research Centre, the Centre for Rural and Remote Mental Health and the Mental Health and Drug and Alcohol Office.
The research described in this article sought to address a key knowledge gap by working in partnership with service providers, consumers and researchers to enhance collaboration between separate MH and AoD services and improve the delivery of care for people who have co-occurring disorders.
Why is integrated care not widely provided as routine care?
There are at least two possible reasons for the lack of sustained uptake of integrated care into routine practice. First, what appears to be missing is a widely-accepted service-delivery model that both adequately reflects best-evidence practice and has the capacity to be tailored to the individual circumstances of different service providers and consumers. Second, it may be that the uptake of integrated care is not being guided by the application of a feasible, acceptable and relevant model of change with which service managers, clinicians and consumers can engage in a meaningful way[CF1] .
At least two preconditions are required for the sustained uptake of IC into routine clinical practice:
- The availability of a treatment model that is standardised based on best-evidence principles, but also able to be tailored to different circumstances;
- The availability of a practical, evidence-based framework to guide services to drive the uptake of IC through the complex transition process.
What did we do?
This study had two aims. First, to co-design and co-implement an evidence-based model of integrated care that could be tailored to multiple services. Second, to construct a pragmatic process for guiding uptake of that model into routine practice.
A mixed-methods approach using Participatory Action Research was implemented in a 20 bed non-acute residential rehabilitation unit for people aged 18 years and over who have been diagnosed with a major mental illness; and an outpatient AoD service for people aged 14 years and over. Participatory Action Research was chosen because it facilitates co-design: a ‘process of collaborative creativity’ in which ideas and thoughts are shared to develop a new product and collectively ‘create new value’ 20. Fifty-six clinicians, five external researchers and ninety-one residents of the rehabilitation unit participated in meetings, surveys or focus groups over four years.
Four cycles of participatory action research were enacted, where existing processes were reviewed, adapted, trialled and adapted again as necessary. Together, participants devised solutions to barriers, and designed logos and posters, manuals and handbooks, and an animated video to introduce newly designed therapeutic groups to consumers. Qualitative and observational data were analysed for emergent themes and self-reported quantitative data were scored on Likert scales.
Booklets designed by clinicians and consumers as handbooks for clinicians and consumers.

A still from a video created by clinicians and played for clients to introduce co-facilitated theraputic group sessions (credit: Dan van der Donk).
Constructing the model and the framework.
Previous studies used logic models to develop treatment frameworks that comprise core components that are evidence-based and are standardised across settings, and flexible activities that are tailored to individual services to operationalise the core components 21-24. This strategy was applied to the development of the service delivery model and the framework described in this article. It is an iterative approach that enables the development of best-evidence models of care that are comparable across different services (the core components) with built-in flexibility to accommodate services’ contexts and preferences (the tailored activities) 23.
What did we find?
A key finding was the importance of embedding a process for monitoring and responding to levels of participation. Engaging staff and consumers in driving their own change process was critical to empowering them to actively lead and achieve change rather than to feel threatened by it. In addition to simply participating in the process, however, the nature of involvement was key. Consistent with Arnstein’s (1969) Ladder of Participation, there was a clear differentiation between seeking input (which can be perceived as tokenistic) and securing active participation (where participants have power to make decisions) 25. Higher levels of control in the change process equate to higher likelihood of achieving change.
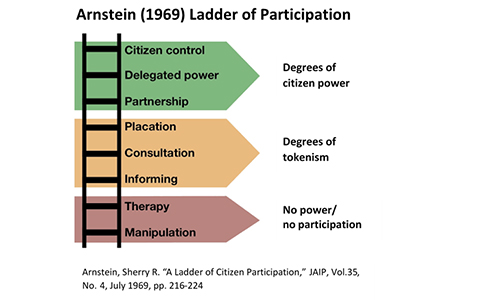
The Ladder of Participation reflects a bottom-up approach, which was described by staff as key to their sense of ownership and ongoing participation:
“…It’s about being asked for input at the beginning of something and to be part of implementing it. I feel like my opinions are being taken seriously and are actually being used.” Norah*, clinician focus group.
Similarly, for consumers, being involved in the development and tailoring of integrated practices was perceived to be ‘welcoming and reassuring’, for example:
“I feel like it’s a really good environment, you know? I like having an opinion and a say in what happens…it’s helped me a lot”. Harry*, consumer focus group.
In contrast, top-down approaches where decisions are imposed, can increase resistance because they are viewed as ‘empty and frustrating’25. The trick, however, is finding the right balance. While bottom-up leadership was key to achieving buy-in and sustainability at a workforce level, top-down leadership was crucial to ensuring relevance and feasibility at an operational level. Clinicians were also unlikely to participate without visible support from their managers.
The Ladder of Participation offers one explanation for the difficulty of achieving effective and sustainable change in clinical settings. That is, participation at all organisational levels is critical, but insufficient attention to the nature and level of that participation prevents the necessary distribution of power between managers, clinicians and consumers to effect real change.
The model and the framework
An agreed, evidence-based service-delivery model and a pragmatic implementation framework were developed (see excerpts, Tables 1 and 2). Involving both a wide range of staff of clinical services and researchers ensured the service-delivery model would represent evidence-based practice by combining the best available research evidence (researchers) with the expertise of service providers and consumers 26. Involving staff from two previously independent service systems (i.e. MH and AoD) encouraged greater alignment between the treatment provided in those systems, and ensured changes were feasible for clinicians to implement. Involving consumers in the development and implementation of the service-delivery model ensured that it would be highly acceptable to consumers and would be more likely to improve the quality of the care that they receive, whilst also upholding their rights to influence and inform the services that are designed to meet their needs27.
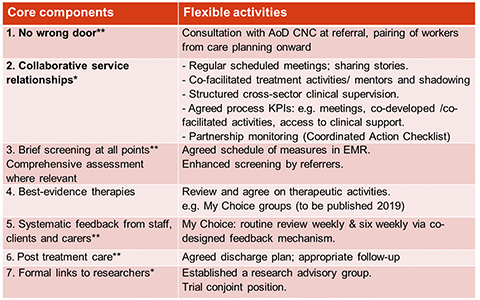
Table 1. The service delivery model. This is an excerpt from the service-delivery model which is expected to be published in early 2019.
Note. All core components are drawn from clinical guidelines. 1 x asterisk = also identified by clinicians, and 2 x asterisks = also identified by clinicians and by consumers.
Ideally, both the model and the framework will now be applied and evaluated in multiple settings and in different countries so that a useful evidence base can be established for the implementation of standardised but adaptable integrated care. Services and policy makers can utilise the model and the framework to increase the uptake of integrated care internationally, or for improved utilisation of the comprehensive range of integrated resources that already exist.
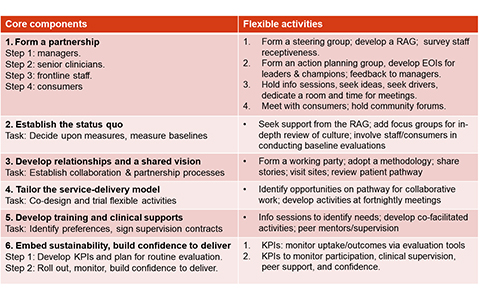
Table 2. The implementation framework. This is an excerpt from the implementation framework which is expected to be published in early 2019.
Conclusion
The sustained uptake of integrated care (or any clinical innovation) is likely to require active participation from frontline staff and consumers, and a practical and feasible systems-change approach to guide the transition process. Attempting to integrate AoD and MH care is a global challenge, but models to facilitate this broader dissemination are most likely to be effective if they emanate from locally driven services, and from resolving real-world problems. A key strength of the service-delivery model and the framework developed here is the standardised but flexible nature of the core components. They provide one possible solution to the challenge of translating integrated care into practice across multiple settings. This pragmatic, clinician-led approach could also be applicable to other services where consumers would benefit from a collaborative approach to care.
About the author
Catherine is a psychologist with a clinical background in substance use, mental health and trauma. She has recently completed her PhD with NDARC, UNSW, and is extending on the work presented here in partnership with NDARC and the Mid North Coast Local Health District.
For further findings and publications from this project, please contact:
Catherine Foley: c.foley@unsw.edu.au
Anthony Shakeshaft: a.shakeshaft@unsw.edu.au








